What have we learned from the COVID-19 pandemic?
April 30, 2022
By Ryan M. Thomas
This month’s newsletter marks a little over two years since the World Health Organization first announced the COVID-19 Pandemic. In February 2020, I remember being in Rome when the first COVID cases were reported. Little did I know that only a few weeks later, the country would be locked down and hospitals would be overflowing with the sick and dying.
As spring is now fully upon us, I’ve decided to focus this month’s newsletter on the positive side. I recently read an article by The New York Times which outlined 14 Lessons For The Next Pandemic.
As someone linked closely to pandemic relief, and who has seen the consequences in my own family, the article really hit home. The piece outlines that we must learn to put data and science first in order to increase preparedness against infectious diseases, to offer equal access to treatment and care, and ultimately, to trust in science. The phrase “trust in science” has unfortunately been politicized and thrown around a lot over the last two years, without getting political, I’ll just say that part of the learning from the last two years is that no party owns science, and unfortunately many health decisions around the world were made from a place of consolidation of power or ideological perspectives instead of evidence-based perspectives.
This Times article also prompted me to think deeper about what we have gained from the COVID-19 Pandemic—while there has been a lot of suffering and death, there were many positive outcomes and learnings as well.
So, where do we go from here?
Today, I am outlining just a few humble thoughts which represent just a tip of the iceberg.
We must increase preparedness.
The pandemic drastically shifted public health response and infrastructure worldwide.
Experts in infectious diseases are concerned that COVID-19 will not be the last novel disease to threaten humanity, but because of changes in climate patterns, advancements of civilization into previously virgin environments, and the increased proximity of humans to animals in agriculture (and wet markets), the opportunity for us to come into contact with novel infectious diseases is increasing.
We might consider that the last two years were an opportunity to test our preparedness to improve our ability for prompt testing, tracking, and robust data analysis. And it has also unveiled that no country has done a great job in preventing or controlling the spread of the SARS-CoV-2 virus.
One of the important lessons from the last two years is that better infrastructure should be readily available for infectious outbreaks.
This learning was outlined in a succinct article by The Guardian. The article notes that the G20 summit called for a global relief fund of up to $15-billion-dollars per year to prepare for COVID-19 relief. It aims to use the funds to tackle public health initiatives like better ventilation systems in office buildings and airplanes to prevent the spread of disease.
There is also a growing consensus to learn from our lack of readiness prior to COVID-19. I won’t go into the negatives in this newsletter, but there are many.
Better preparedness is especially important since new studies show that historically, pandemics have been much more common and that the risk for a pandemic has increased more than three-fold over the last several years.
We must push the boundaries of healthcare to rapidly and effectively respond to new threats and pivot when data presents better information.
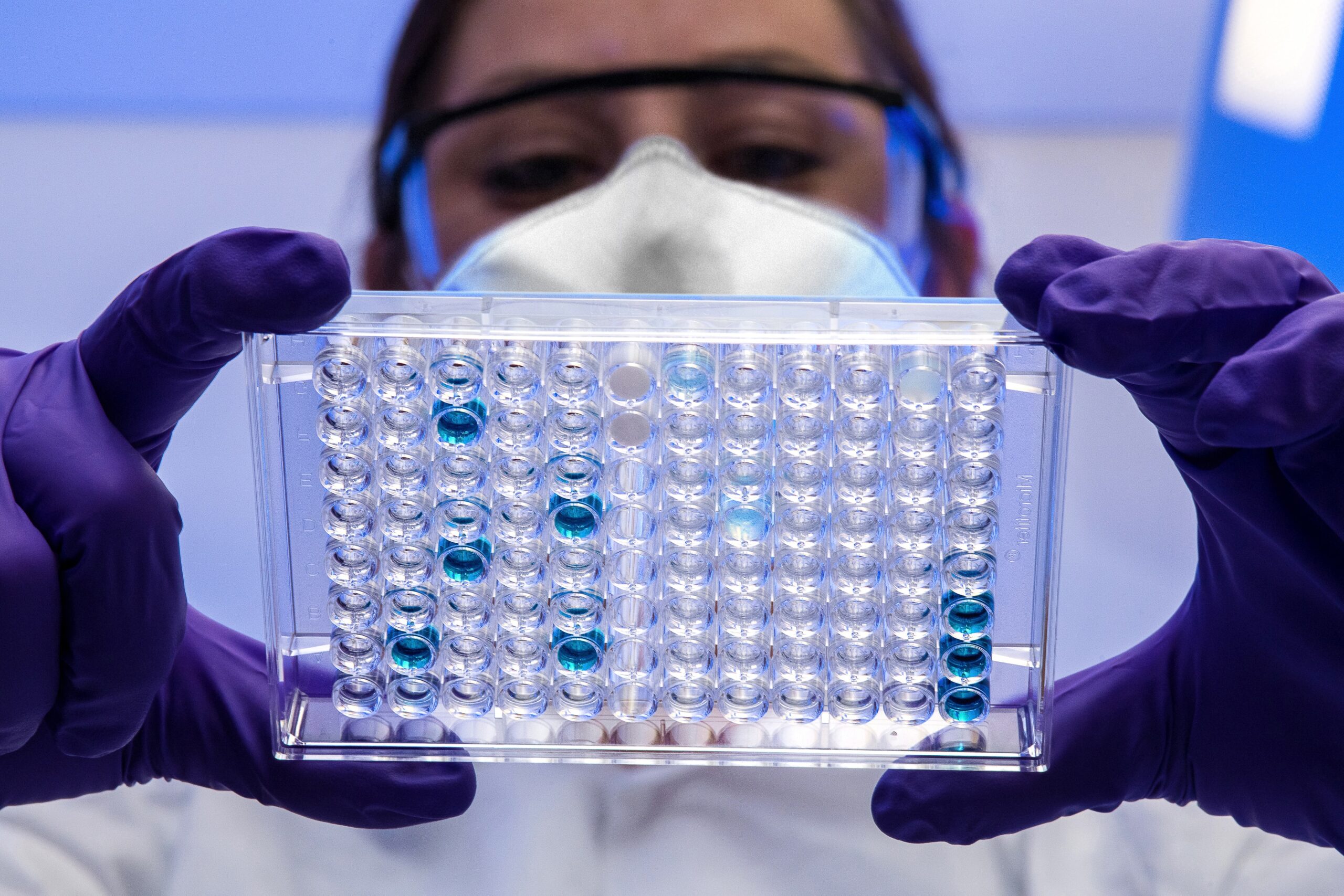
In light of the COVID-19 Pandemic, we have also seen the rise of new and innovative diagnostic testing, which are proving to be the fastest, most cost effective and accurate tools of their kind in history.
When it comes to manufacturing and the development of vaccines and treatments, we know that Operation Warp Speed evolutionized the way in which COVID-19 vaccines are designed, developed, and distributed.
Faster and more voluminous than ever before, this novel partnership between public-private spheres in the United States allowed for the rapid distribution of COVID-19 diagnostics, therapeutics, and vaccines, and the fastest-to-market program ever in the United State’s history.
And at Eyam, we have incorporated many of these learnings – and improved upon the missteps of others to revolutionize the speed and sophistication of vaccine design. We continue to be advocates of localized manufacturing facilities in the development of Eyam’s SARS-CoV-2 vaccines, and we’ve also learned to address the downfalls of existing, first-generation vaccines.
We must advocate for the democratization of vaccines.
Another key learning that has been brought to the forefront as a consequence of the COVID-19 Pandemic is the health inequality endured by communities across the globe, which The Lancet has coined, the global access gap.
Low-income and middle-income families worldwide have less access to medical treatment and prevention measures. With lower levels of preventative measures, the immunocompromised have a reported four-times higher mortality rate in low-income countries compared to high-income countries
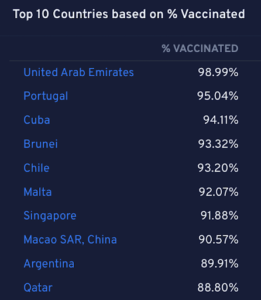
Figure 1: Top 10 Countries with Most Vaccinated Population in %
Source: https://covid19.pemandu.org/#
The Lancet also spoke about the Rotavirus vaccine, which was approved by the World Health Organization in 2009 for worldwide immunization. This initiative resulted in an almost immediate uptake of 70% in the USA—yet adversely, as reported in 2020, only 40% of children received 3-doses, globally.
There are several challenges to democratizing access to vaccines. The first hurdle is cost. Vaccines need to be made available to countries at a reasonable cost based upon the resources available. Part of the challenge is that vaccines are often manufactured a great distance from the receiving country, making shipping costly.
During the process of shipping and distribution, many vaccines – like Pfizer’s COVID-19 vaccine – have to be stored at temperatures of up to -90*C. Special ultra-cold freezers must be used to transport the vaccines to preserve their ability to effectively protect recipients. These costs – and extra measures – make it challenging to get vaccines to remote areas with fewer financial resources.
One solution, in development by Eyam, has been to develop a vaccine platform in which the manufacturing of vaccines requires fewer raw materials, less capital intensive machinery, and is stable at higher temperatures effectively reducing the cost of transporting and delivering vaccines.
This solution also encourages developing countries to take back control of their health care system with better access to preventive vaccines, and allows for the licensing of vaccine technologies to be able to manufacture in-country.
We must advocate for transparency and the dissemination of trustworthy information.
Trustworthiness has been a key learning throughout the pandemic. And I recently came across a Forbes interview, titled a Biotech Pioneer On Lessons Learned From The Pandemic, where the interviewee speaks to how the media has shaped and evolved in light of the global crisis.
He discusses the rise of disinformation online—and the phenomenon of self-medication by way of the internet.
There are pros and cons to the phenomenon of self-medication. On one hand, it shows an increase in responsibility for one’s own health. On the other hand, it can displace or replace the professional evaluation and treatment of medical professionals leading to an increase in unintended overdoses, toxicity, and antagonist drug interactions.
This “Self-Health Movement,” as I like to call it, is a consequence of many factors, but one factor that seems quite clear to me is the distrust towards public health officials.
I don’t intend to downplay the role of bad actors or misinformation here, but rather to point out that a lack of transparency and inconsistent messaging from our public health officials is one factor that led to an increase in distrust and vaccine hesitancy amongst an increasing proportion of the population.
While operating at the onset of the pandemic, with little information about a novel virus is no small task, the overly politicized environment in which we live makes for a challenging environment to communicate a clear and consistent message.
One important lesson that I think should be taken into consideration is that even messaging with good intentions, but with a lack of transparency is counterproductive. The task of motivating billions of people to get vaccinated and protected against COVID-19 in less than a year was a task of monumental proportions. Massaging data, changing definitions and downplaying certain short-comings of the first generation vaccines were exposed and exploited, creating greater distrust and threatening the long-term adoption of vaccines that have ultimately been one of the greatest life saving technologies ever created.
What struck me about the Forbes article was the quote, “science is something that has a hypothesis. You test the data and you reach a conclusion based solely on the results of the science.”
Going forward, transparency of data needs to be made more available to the public. Of course, the interpretation of data is critical, but in the vacuum of scientific data and support, superstition thrives.
We must continue to lead with science.
I am a firm believer that we must learn from history. After all, science depends on it.
Eyam cannot control many things I have mentioned above: public health relief initiatives, the mechanics and the monitoring of viruses, or even public health policies— but we can continue the development of safe, efficacious, and scalable vaccine solutions for a number of life-threatening diseases, to offer protection for all.
What have we learned from the COVID-19 pandemic?
April 30, 2022
By Ryan M. Thomas
This month’s newsletter marks a little over two years since the World Health Organization first announced the COVID-19 Pandemic. In February 2020, I remember being in Rome when the first COVID cases were reported. Little did I know that only a few weeks later, the country would be locked down and hospitals would be overflowing with the sick and dying.
As spring is now fully upon us, I’ve decided to focus this month’s newsletter on the positive side. I recently read an article by The New York Times which outlined 14 Lessons For The Next Pandemic.
As someone linked closely to pandemic relief, and who has seen the consequences in my own family, the article really hit home. The piece outlines that we must learn to put data and science first in order to increase preparedness against infectious diseases, to offer equal access to treatment and care, and ultimately, to trust in science. The phrase “trust in science” has unfortunately been politicized and thrown around a lot over the last two years, without getting political, I’ll just say that part of the learning from the last two years is that no party owns science, and unfortunately many health decisions around the world were made from a place of consolidation of power or ideological perspectives instead of evidence-based perspectives.
This Times article also prompted me to think deeper about what we have gained from the COVID-19 Pandemic—while there has been a lot of suffering and death, there were many positive outcomes and learnings as well.
So, where do we go from here?
Today, I am outlining just a few humble thoughts which represent just a tip of the iceberg.
We must increase preparedness.
The pandemic drastically shifted public health response and infrastructure worldwide.
Experts in infectious diseases are concerned that COVID-19 will not be the last novel disease to threaten humanity, but because of changes in climate patterns, advancements of civilization into previously virgin environments, and the increased proximity of humans to animals in agriculture (and wet markets), the opportunity for us to come into contact with novel infectious diseases is increasing.
We might consider that the last two years were an opportunity to test our preparedness to improve our ability for prompt testing, tracking, and robust data analysis. And it has also unveiled that no country has done a great job in preventing or controlling the spread of the SARS-CoV-2 virus.
One of the important lessons from the last two years is that better infrastructure should be readily available for infectious outbreaks.
This learning was outlined in a succinct article by The Guardian. The article notes that the G20 summit called for a global relief fund of up to $15-billion-dollars per year to prepare for COVID-19 relief. It aims to use the funds to tackle public health initiatives like better ventilation systems in office buildings and airplanes to prevent the spread of disease.
There is also a growing consensus to learn from our lack of readiness prior to COVID-19. I won’t go into the negatives in this newsletter, but there are many.
Better preparedness is especially important since new studies show that historically, pandemics have been much more common and that the risk for a pandemic has increased more than three-fold over the last several years.
We must push the boundaries of healthcare to rapidly and effectively respond to new threats and pivot when data presents better information.
In light of the COVID-19 Pandemic, we have also seen the rise of new and innovative diagnostic testing, which are proving to be the fastest, most cost effective and accurate tools of their kind in history.
When it comes to manufacturing and the development of vaccines and treatments, we know that Operation Warp Speed evolutionized the way in which COVID-19 vaccines are designed, developed, and distributed.
Faster and more voluminous than ever before, this novel partnership between public-private spheres in the United States allowed for the rapid distribution of COVID-19 diagnostics, therapeutics, and vaccines, and the fastest-to-market program ever in the United State’s history.
And at Eyam, we have incorporated many of these learnings – and improved upon the missteps of others to revolutionize the speed and sophistication of vaccine design. We continue to be advocates of localized manufacturing facilities in the development of Eyam’s SARS-CoV-2 vaccines, and we’ve also learned to address the downfalls of existing, first-generation vaccines.
We must advocate for the democratization of vaccines.
Another key learning that has been brought to the forefront as a consequence of the COVID-19 Pandemic is the health inequality endured by communities across the globe, which The Lancet has coined, the global access gap.
Low-income and middle-income families worldwide have less access to medical treatment and prevention measures. With lower levels of preventative measures, the immunocompromised have a reported four-times higher mortality rate in low-income countries compared to high-income countries
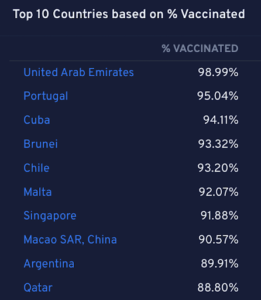
Figure 1: Top 10 Countries with Most Vaccinated Population in %
Source: https://covid19.pemandu.org/#
The Lancet also spoke about the Rotavirus vaccine, which was approved by the World Health Organization in 2009 for worldwide immunization. This initiative resulted in an almost immediate uptake of 70% in the USA—yet adversely, as reported in 2020, only 40% of children received 3-doses, globally.
There are several challenges to democratizing access to vaccines. The first hurdle is cost. Vaccines need to be made available to countries at a reasonable cost based upon the resources available. Part of the challenge is that vaccines are often manufactured a great distance from the receiving country, making shipping costly.
During the process of shipping and distribution, many vaccines – like Pfizer’s COVID-19 vaccine – have to be stored at temperatures of up to -90*C. Special ultra-cold freezers must be used to transport the vaccines to preserve their ability to effectively protect recipients. These costs – and extra measures – make it challenging to get vaccines to remote areas with fewer financial resources.
One solution, in development by Eyam, has been to develop a vaccine platform in which the manufacturing of vaccines requires fewer raw materials, less capital intensive machinery, and is stable at higher temperatures effectively reducing the cost of transporting and delivering vaccines.
This solution also encourages developing countries to take back control of their health care system with better access to preventive vaccines, and allows for the licensing of vaccine technologies to be able to manufacture in-country.
We must advocate for transparency and the dissemination of trustworthy information.
Trustworthiness has been a key learning throughout the pandemic. And I recently came across a Forbes interview, titled a Biotech Pioneer On Lessons Learned From The Pandemic, where the interviewee speaks to how the media has shaped and evolved in light of the global crisis.
He discusses the rise of disinformation online—and the phenomenon of self-medication by way of the internet.
There are pros and cons to the phenomenon of self-medication. On one hand, it shows an increase in responsibility for one’s own health. On the other hand, it can displace or replace the professional evaluation and treatment of medical professionals leading to an increase in unintended overdoses, toxicity, and antagonist drug interactions.
This “Self-Health Movement,” as I like to call it, is a consequence of many factors, but one factor that seems quite clear to me is the distrust towards public health officials.
I don’t intend to downplay the role of bad actors or misinformation here, but rather to point out that a lack of transparency and inconsistent messaging from our public health officials is one factor that led to an increase in distrust and vaccine hesitancy amongst an increasing proportion of the population.
While operating at the onset of the pandemic, with little information about a novel virus is no small task, the overly politicized environment in which we live makes for a challenging environment to communicate a clear and consistent message.
One important lesson that I think should be taken into consideration is that even messaging with good intentions, but with a lack of transparency is counterproductive. The task of motivating billions of people to get vaccinated and protected against COVID-19 in less than a year was a task of monumental proportions. Massaging data, changing definitions and downplaying certain short-comings of the first generation vaccines were exposed and exploited, creating greater distrust and threatening the long-term adoption of vaccines that have ultimately been one of the greatest life saving technologies ever created.
What struck me about the Forbes article was the quote, “science is something that has a hypothesis. You test the data and you reach a conclusion based solely on the results of the science.”
Going forward, transparency of data needs to be made more available to the public. Of course, the interpretation of data is critical, but in the vacuum of scientific data and support, superstition thrives.
We must continue to lead with science.
I am a firm believer that we must learn from history. After all, science depends on it.
Eyam cannot control many things I have mentioned above: public health relief initiatives, the mechanics and the monitoring of viruses, or even public health policies— but we can continue the development of safe, efficacious, and scalable vaccine solutions for a number of life-threatening diseases, to offer protection for all.